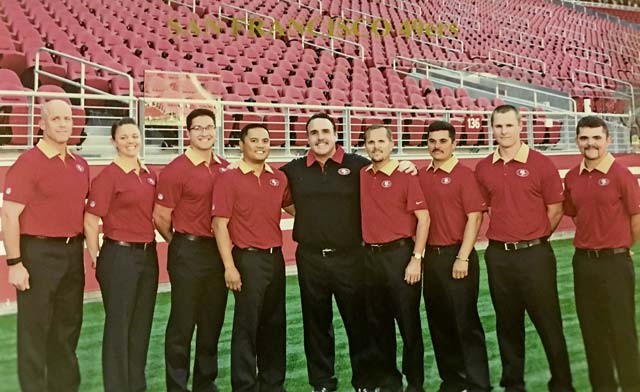
Army Physician Assistant Capt. Tyson Baynes (left) joins members of the San Francisco 49ers Medical Staff during his Training with Industry assignment. To his left are Certified Athletic Trainer Laura Schnettgoecke, Physical Therapist Ryan Donahue, Certified Athletic Trainer Manny Rivera, 49ers Head Coach Jim Tomsula, Head Athletic Trainer Jeff Ferguson, and Certified Athletic Trainers Ray Martinez, Iain Mistrot Bart Jamison.
If you’re in the military, you’ve more than likely attended required annual training that covers traumatic brain injuries. You’ve learned that an individual who has sustained a concussion and not recovered isn’t at full operating capacity.
If the individual is a service member, this could cause a degradation in unit readiness and impact the mission. We have learned a lot in the last decade about TBIs, but there is much we do not know.
The Department of Defense and the Army are dedicated to providing the most thorough care to service members and their families that have sustained head injuries in order to reduce residual effects and minimize the impact on mission.
The Army has teamed up with various military and civilian organizations, such as the National Football League, to research and develop best practices regarding the care of TBIs and musculoskeletal injuries.
As part of the continued effort, Army Medical Department and the Specialty Corps developed a “Training with Industry” program offered through Long Term Health Education and Training.
The Army Specialty Corps pairs an officer with the NFL for a year to where he or she is fully integrated with team medical staff with the goal of collaborating and bringing the best practices back to the Army and ultimately improving care of the Soldier Athlete.
In the following paragraphs, I will summarize my incredible experience with the San Francisco 49ers by providing an overview of the NFL’s procedures regarding their handling of concussions and the similarities with the Army’s TBI polices.
Before I go into my experience with the 49ers, I’ll share how I became interested in concussion care. After returning from a deployment in Afghanistan in 2012, I assisted with medical reverse Soldier Readiness Processing at my unit at the Baumholder Health Clinic. One of the tasks of Soldier Readiness Processing was conducting TBI screenings.
I worked closely with a TBI nurse case manager. Through her efforts, I was able to appreciate how complex concussions can be and that many symptoms overlap with multiple disease processes. I came to enjoy the clinical and academic challenges the field offers and sought occasions for self improvement. Prior to joining the 49ers, I had the privilege to assist at the Landstuhl Regional Medical Center TBI Clinic.
I spent as much time as possible learning from the incredibly passionate staff members at the clinic. It was during this time I increased the skills needed to assess the concussed patient’s reported history while at the same time conducting a detailed physical exam. Working LRMC TBI Clinic has opened many doors of opportunities to not only improve my professional skills but more importantly, deliver quality care to our Soldier Athletes.
I was fortunate to be selected for the 2015-2016 Training with Industry and subsequently assigned to the 49ers. Working with the team for the past eight months, I’ve experienced firsthand the actions and effects of a well-integrated and synchronized sports medicine team. The relationship between the sports med department and the team administration is similar to the battalion-brigade-division medical sections and their respective command and staff.
Much like military units that are in a deployment train-up cycle, the NFL has phases of training prior to the start of the regular season, with the culminating training event being the preseason games. The NFL preseason can be compared to Joint Readiness Training Rotation or National Training Center rotations, which military units rotate through prior to their deployment.
Since the start of training camp in August 2015 and until the end of the season in January 2016, the medical staff started most mornings at 6:30 a.m. On average, days were long and ended at 7 p.m., six days a week. Game day could be shorter or longer depending on kickoff time and if the game was home or away.
This grind is very similar to deployments or extended field problems, except that the stakes for the military could be a matter life and death. Just as it’s important to maintain Soldiers health on the battlefield, it was incumbent on the 49er’s medical staff to quickly, but thoroughly, evaluate player injuries and illnesses in order to determine a disposition, such as Return to Participation; RTP with limitations, similar to the activity limiting profile; or rehabilitation activities.
The team medical staff is in constant contact with the coaching staff, strength and conditioning coordinators, and the nutritional staff so that every aspect of the athletes training is modified specifically to their injury. This ensures that over training or under training does not occur and that the player is healthy in order to return to play.
Regarding concussions, rules for the NFL have changed to make for safer competition. However, due to the nature of the sport, a few concussions occurred during the season. It was interesting to see that because of the NFL’s increased awareness of concussions and focused education on the injury. The culture is changing to the point that players are less likely to play through a head injury.
In the event the medical staff, team staff or officiating crew didn’t recognize a possible TBI had occurred, players would alert the medical staff when they’ve suspected fellow teammates were concussed. In some case, the injured players self reported. This model of awareness and education mirrors the U.S. Army Medical Department’s TBI policy goals.
If a player was suspected of having a concussion, an unaffiliated neurologist and team physician would review the potential concussive event via sideline monitors. The medical staff would then ask the player a battery of questions to determine if the player was oriented to person, place and time and to determine if the player was experiencing symptoms related to the hit.
If at that time it was determined that the player was symptomatic, the player was escorted into the locker room where a comprehensive cognitive and neurological exam was conducted using the X2, which is a combination the Sport Concussion Assessment Test and NFL specific history. Of note, the SCAT is similar to the military’s Military Acute Concussion Evaluation.
After a diagnosis of concussion was given, I would follow the player through their recovery process, which included visiting an NFL-appointed neurologist — independent from the team — who would recommend continued treatment or clearance for the initiation of exertional activities.
Much like the Army’s Return to Duty concussion protocol, the NFL has developed and implemented a stringent RTP protocol, which is a stepwise progression of physical and mental activity. The player is considered RTP only after he is asymptomatic and neurocognitive testing has returned back to baseline.
At the onset of a NFL training camp, the roster contains 90 players. At the conclusion of camp, only 53 names remain on the active roster and 10 players are assigned to the practice squad. The 53 man active roster and the 10 man practice squad is a NFL mandated number.
The reality of a limited number of athletes available to play a physically intense and grueling 16 game schedule makes it extremely important that the medical staff provides injury prevention techniques and conducts baseline neurocognitive testing to determine the brain health of a player prior to contact.
When injuries occur, it’s paramount that the players receive world class medical care to ensure a healthy and timely return in order to continue mission. As a midlevel medical provider in the military, I realize our Soldier athletes have high physical and mental demands placed on them.
Each Soldier athlete is a member of a team that is counting on them to fulfill their assignment. It’s critical that our Soldier athletes receive the best prevention techniques available to decrease risk of injury. When the Soldier athlete becomes injured, it is the medical communities responsibility to provide evidence-based, best-practiced medical care that increases the service member’s chances to recover and influence overall mission success.
This objective will continue to be the point of focus during the remainder of my time in the Training with Industry program, with the intent of contributing to Army medicine as we transition to the medical modal of Systems for Health in order to sustain the health of the war fighter.


